When facing bacterial infections, few classes of antibiotics offer the versatile middle ground quite like second-generation cephalosporins. These powerful medications serve as crucial tools in a clinician's arsenal, demonstrating a unique balance in their Clinical Indications & Therapeutic Uses of 2nd Gen Cephalosporins that makes them invaluable for a range of conditions, from respiratory woes to complex surgical scenarios. Understanding when and why to reach for these antibiotics is key to effective patient care.
At a Glance: Key Takeaways on Second-Generation Cephalosporins
- Mechanism of Action: They target and inhibit bacterial cell wall synthesis, leading to bacterial death.
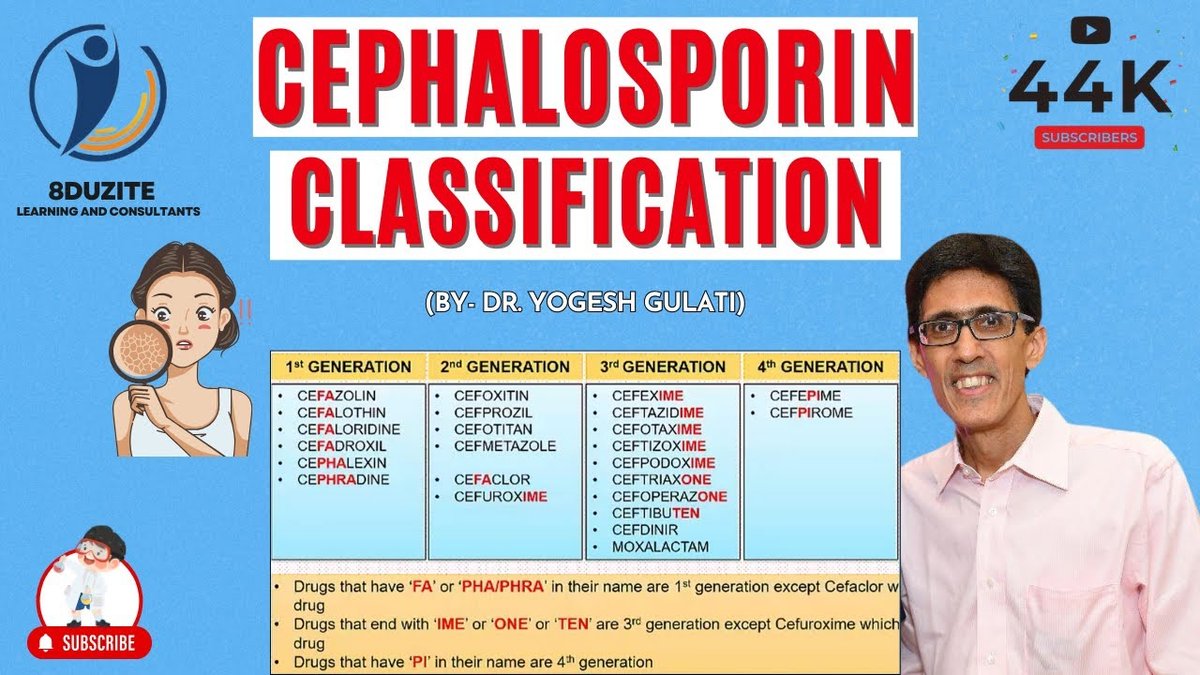
- Spectrum of Activity: Broader gram-negative coverage than first-gen cephalosporins, with slightly less potency against gram-positives. Notable for covering H. influenzae, E. coli, and Klebsiella pneumoniae. Cephamycins (like cefoxitin and cefotetan) specifically tackle Bacteroides species.
- Common Uses: Effective for lower respiratory tract infections, skin and soft tissue infections, urinary tract infections, gynecological infections, intra-abdominal infections, and some bone and joint infections.
- Key Names: Cefaclor, Cefotetan, Cefoxitin, Cefprozil, Cefuroxime (parenteral), Cefuroxime axetil (oral), and Loracarbef are the main players.
- Considerations: Dosage adjustments are often needed for renal impairment. Hypersensitivity reactions are a potential, albeit rare, serious side effect.
Unpacking Second-Generation Cephalosporins: What Makes Them Tick?
Imagine a family of antibiotics, each generation evolving to tackle slightly different bacterial challenges. Second-generation cephalosporins represent a significant step up from their first-generation predecessors, offering an expanded spectrum of activity that addresses a wider range of Gram-negative bacteria while retaining some Gram-positive coverage.
Derived from the mold Acremonium, these antibiotics work by cleverly interfering with a bacterium's ability to build its protective cell wall. They accomplish this by binding to specific proteins within the bacterial wall, known as penicillin-binding proteins (PBPs), through their beta-lactam rings. This disruption leads to a fatally flawed cell wall, causing the bacteria to lyse and die. It's a precise and effective way to halt an infection in its tracks.
While generally less potent against Gram-positive bacteria than their first-gen cousins, second-gen cephalosporins shine against a particular set of Gram-negative offenders. You'll often find them effective against common culprits like Haemophilus influenzae, Enterobacter aerogenes, some Neisseria species, Proteus mirabilis, Escherichia coli, and Klebsiella pneumoniae.
A notable distinction within this group lies with the cephamycins, such as cefoxitin and cefotetan. These specific agents offer enhanced coverage against anaerobic bacteria, particularly Bacteroides species, making them crucial for infections where these organisms are likely involved, such as intra-abdominal or gynecological conditions.
Why Opt for a Second-Gen Cephalosporin? Their Broad Therapeutic Reach
Second-generation cephalosporins aren't just an option; they're often a preferred choice for their efficacy across a diverse array of infections. When you need an antibiotic that covers a good mix of Gram-positive and, especially, Gram-negative bacteria, these drugs frequently fit the bill. Their versatility makes them suitable for treating infections in various bodily systems.
Common scenarios where these antibiotics excel include:
- Bone and Joint Infections: Tackling bacterial invaders in deeper tissues.
- Skin and Soft Tissue Infections: From cellulitis to more complex skin conditions.
- Gynecological Infections: Addressing pelvic inflammatory disease or endometritis.
- Intra-abdominal Infections: Particularly those involving anaerobes, thanks to agents like cefoxitin and cefotetan.
- Lower Respiratory Tract Infections: Such as pneumonia or acute exacerbations of chronic bronchitis.
- Serious Urinary Tract Infections: Including pyelonephritis (kidney infections).
- Meningitis in Children: Specific agents like cefuroxime can be used.
- Blood Infections (Septicemia): When appropriate for the identified pathogens.
To truly appreciate the nuances and specific applications across this class, it's beneficial to explore 2nd Generation Cephalosporins in more detail. Each drug brings its own unique strengths to the table, and selecting the right one depends heavily on the specific infection, the suspected pathogens, and patient-specific factors.
Diving Deeper: Specific Second-Generation Cephalosporins and Their Unique Roles
While they share a family name, each second-generation cephalosporin has its own distinct microbiological profile and a set of preferred clinical indications. Let's break down the key players you'll encounter.
Cefaclor (Ceclor®): A Go-To for Common Infections
Cefaclor is an oral second-generation cephalosporin often prescribed for a variety of community-acquired infections.
Microbiology:
Cefaclor is bactericidal, working by inhibiting bacterial cell-wall synthesis. It's active against several Gram-positive aerobes, including Staphylococci (even some penicillinase-producing strains), Streptococcus pneumoniae, and S. pyogenes. On the Gram-negative side, it covers E. coli, H. influenzae (with a crucial caveat), Klebsiella spp., and P. mirabilis. It also has some activity against Gram-positive anaerobes like Bacteroides spp. (excluding B. fragilis), Peptococcus, Peptostreptococcus, and Propionibacterium acnes.
However, it's important to note its resistances: Pseudomonas spp., Acinetobacter calcoaceticus, most Enterococcus spp., Enterobacter spp., indole-positive Proteus, Morganella morganii, Providencia rettgeri, and Serratia spp. are typically not susceptible. Staphylococci resistant to methicillin-type antibiotics will also exhibit cross-resistance to cefaclor.
Indications:
Cefaclor is commonly indicated for:
- Otitis media (middle ear infections)
- Lower respiratory tract infections, including pneumonia
- Pharyngitis and tonsillitis (strep throat)
- Urinary tract infections (both pyelonephritis and cystitis)
- Skin and skin structure infections
Actionable Insights for Cefaclor: - H. influenzae Resistance: Be aware that beta-lactamase-negative ampicillin-resistant (BLNAR) strains of H. influenzae are resistant to cefaclor. Susceptibility testing is crucial if these strains are suspected.
- S. pyogenes: While active, penicillin remains the preferred drug for S. pyogenes infections. Cefaclor's efficacy in preventing rheumatic fever following strep throat has not been established. Use is based on organism susceptibility.
- Duration: For β-hemolytic streptococcal infections, therapy should continue for at least 10 days to ensure eradication.
Dosage & Administration (Oral): - Adults: The usual dose is 250 mg every 8 hours. For severe infections or less susceptible organisms, this dosage may be doubled.
- Pediatric (usual): 20 mg/kg/day, divided into doses given every 8 hours. For serious infections, otitis media, or less susceptible organisms, the dose can increase to 40 mg/kg/day, with a maximum of 1 gram per day.
- Pediatric (BID option): For otitis media and pharyngitis, the total daily dosage can be divided and given every 12 hours.
- Renal Impairment: Dosage adjustments are generally not required for renal impairment, but always confirm with current guidelines and patient-specific factors.
Cefotetan: Targeting Anaerobes and Surgical Prophylaxis
Cefotetan is a potent parenteral (IV or IM) second-generation cephalosporin known for its excellent stability against beta-lactamases and significant activity against anaerobic bacteria.
Microbiology:
Cefotetan is bactericidal, effectively inhibiting bacterial cell wall synthesis. A key feature is its high stability against beta-lactamases, largely due to a unique methoxy group in its structure. It boasts a wide spectrum against aerobic and anaerobic Gram-positive and Gram-negative organisms. This includes E. coli, H. influenzae (even ampicillin-resistant strains), Klebsiella spp., S. aureus (including penicillinase-producing), S. pyogenes, and importantly, Bacteroides fragilis and other Bacteroides spp.
Resistances include approximately half of Enterobacter spp., most Pseudomonas aeruginosa and Acinetobacter spp., methicillin-resistant staphylococci, and most Enterococcus spp.
Indications:
Cefotetan's broad spectrum makes it suitable for:
- Urinary tract infections
- Lower respiratory tract infections
- Skin and skin structure infections
- Gynecologic infections (e.g., pelvic inflammatory disease)
- Intra-abdominal infections (e.g., peritonitis, appendicitis)
- Bone and joint infections
It is also widely used for preoperative prophylaxis in clean-contaminated or potentially contaminated surgeries, such as cesarean section, hysterectomy, biliary tract surgery, and gastrointestinal surgery, due to its excellent anaerobic coverage.
Actionable Insights for Cefotetan: - Chlamydia: Cefotetan has no activity against Chlamydia trachomatis. If chlamydial coinfection is suspected in gynecologic infections, appropriate antichlamydial coverage must be added.
- Aminoglycoside Co-administration: Monitor renal function closely if cefotetan is administered concomitantly with aminoglycosides, as there is a potential for increased nephrotoxicity.
Dosage & Administration (IV or IM): - Adults (General Treatment): The usual dose is 1-2 grams every 12 hours. The maximum daily dosage is 6 grams.
- Prophylaxis: A single dose of 1-2 grams IV, given 30-60 minutes prior to surgery. For cesarean section, administer after the umbilical cord is clamped.
Renal Dosing (Adults, based on Creatinine Clearance, CrCl): - CrCl > 30 mL/min: Usual dosage every 12 hours.
- CrCl 10-30 mL/min: Usual dosage every 24 hours, OR half the usual dose every 12 hours.
- CrCl < 10 mL/min: Usual dosage every 48 hours, OR one-quarter of the usual dose every 12 hours.
- Hemodialysis: Administer one-quarter of the usual recommended dose every 24 hours on days between dialysis sessions, and one-half of the usual recommended dose on the day of dialysis.
Cefoxitin (Mefoxin®): The Surgical Workhorse with Broad Anaerobic Power
Cefoxitin is another powerful parenteral cephamycin, highly valued for its exceptional stability against beta-lactamases and its robust activity against a wide range of anaerobic bacteria, especially Bacteroides fragilis.
Microbiology:
Like cefotetan, cefoxitin is bactericidal and inhibits bacterial cell wall synthesis. It exhibits high stability against beta-lactamases, allowing it to remain effective against many resistant strains. Its spectrum covers aerobic Gram-positive bacteria (S. aureus [including penicillinase-producing], S. epidermidis, S. agalactiae, S. pneumoniae, S. pyogenes), and a host of aerobic Gram-negative bacteria (E. coli, H. influenzae, Klebsiella spp., M. morganii, N. gonorrhoeae [including penicillinase-producing], P. mirabilis, P. vulgaris, Providencia spp.). Crucially, it's highly active against anaerobic Gram-positive (Clostridium spp., Peptococcus niger, Peptostreptococcus spp.) and anaerobic Gram-negative bacteria, including the notoriously difficult Bacteroides spp., particularly B. fragilis.
Resistances include methicillin/oxacillin-resistant staphylococci, most Enterococcus spp., most Pseudomonas aeruginosa, and many Enterobacter cloacae.
Indications:
Cefoxitin is indicated for the treatment of serious infections, including:
- Lower respiratory tract infections
- Urinary tract infections
- Intra-abdominal infections
- Gynecological infections
- Septicemia (blood infections)
- Bone and joint infections
- Skin and skin structure infections
It is also a go-to for prophylaxis in various surgeries, particularly those involving the gastrointestinal tract (uncontaminated), vaginal or abdominal hysterectomy, and cesarean section, where its anaerobic coverage is a significant advantage.
Actionable Insights for Cefoxitin: - Chlamydia: Cefoxitin does not cover Chlamydia trachomatis. If chlamydial infection is suspected, additional appropriate antichlamydial therapy should be administered.
- Group A Strep: For infections caused by group A beta-hemolytic streptococci, therapy should be maintained for at least 10 days to prevent complications like rheumatic fever.
- Pus Collections: Surgical drainage should always be considered and performed for significant collections of pus where indicated, as antibiotics alone may not be sufficient.
Dosage & Administration (IV): - Adults (Treatment): The usual range is 1-2 grams every 6 to 8 hours. For very severe infections (e.g., gas gangrene), the maximum can be up to 12 grams daily.
- Adults (Prophylaxis): A 2-gram IV dose just prior to surgery, followed by 2 grams every 6 hours after the initial dose for no more than 24 hours. For cesarean section, a single 2-gram dose at umbilical cord clamping, OR a three-dose regimen (2 grams at cord clamping, then 2 grams at 4 and 8 hours post-initial dose).
- Pediatric (3 months and older): 80-160 mg/kg/day divided into four to six equal doses. Higher doses may be used for severe infections, but the total daily dosage should not exceed 12 grams.
- Pediatric (Prophylaxis 3 months+): 30-40 mg/kg at the same intervals designated for adults.
Renal Dosing (Adults):
An initial loading dose of 1-2 grams is recommended. - CrCl 50-30 mL/min: 1-2 grams every 8-12 hours.
- CrCl 29-10 mL/min: 1-2 grams every 12-24 hours.
- CrCl 9-5 mL/min: 0.5-1 gram every 12-24 hours.
- CrCl < 5 mL/min: 0.5-1 gram every 24-48 hours.
- Hemodialysis: A loading dose of 1-2 grams should be administered after each hemodialysis session, followed by the appropriate maintenance dose.
Cefprozil (Cefzil®): Oral Option for Respiratory and Skin Infections
Cefprozil is an oral second-generation cephalosporin frequently chosen for its effectiveness in treating mild to moderate infections, particularly those affecting the respiratory tract and skin.
Indications:
Cefprozil is indicated for the treatment of mild to moderate infections in:
- Upper Respiratory Tract:
- Pharyngitis/tonsillitis caused by S. pyogenes.
- Otitis media caused by S. pneumoniae, H. influenzae (including beta-lactamase-producing strains), and M. catarrhalis (including beta-lactamase-producing strains).
- Acute sinusitis caused by S. pneumoniae, H. influenzae (including beta-lactamase-producing strains), and M. catarrhalis (including beta-lactamase-producing strains).
- Lower Respiratory Tract:
- Secondary bacterial infection of acute bronchitis.
- Acute bacterial exacerbation of chronic bronchitis, caused by S. pneumoniae, H. influenzae (including beta-lactamase-producing strains), and M. catarrhalis (including beta-lactamase-producing strains).
- Skin and Skin Structure:
- Uncomplicated skin and skin-structure infections caused by S. aureus (including penicillinase-producing strains) and S. pyogenes.
Actionable Insights for Cefprozil: - Surgical Drainage: As with many skin infections, abscesses usually require surgical drainage in addition to antibiotic therapy for effective resolution.
- S. pyogenes: While effective, penicillin is generally considered the usual drug of choice for S. pyogenes infections.
Dosage & Administration (Oral): - Adults (13 years and older):
- Pharyngitis/Tonsillitis: 500 mg once daily for 10 days.
- Acute Sinusitis: 250 mg or 500 mg every 12 hours for 10 days (higher dose for moderate to severe infections).
- Bronchitis: 500 mg every 12 hours for 10 days.
- Uncomplicated Skin/Skin Structure: 250 mg every 12 hours, or 500 mg every 24 hours, or 500 mg every 12 hours for 10 days.
- Children (2-12 years):
- Pharyngitis/Tonsillitis: 7.5 mg/kg every 12 hours for 10 days.
- Uncomplicated Skin/Skin Structure: 20 mg/kg every 24 hours for 10 days.
- Infants & Children (6 months-12 years):
- Otitis Media: 15 mg/kg every 12 hours for 10 days.
- Acute Sinusitis: 7.5 mg/kg or 15 mg/kg every 12 hours for 10 days (higher dose for moderate to severe infections).
- Duration: For Streptococcus pyogenes infections, therapy should be for at least 10 days. The recommended adult doses should not be exceeded.
Renal Dosing (Adults, based on CrCl): - CrCl 30-120 mL/min: Standard dosage and dosing interval.
- CrCl 0-29 mL/min: 50% of the standard dose at the standard dosing interval.
- Hemodialysis: Administer after the completion of hemodialysis.
Cefuroxime (Zinacef® - Parenteral): Versatility for Serious Hospital-Acquired Infections
Cefuroxime, in its parenteral form (Zinacef®), is a highly stable and versatile second-generation cephalosporin, often employed in hospital settings for its broad coverage and ability to tackle more serious infections, including meningitis.
Microbiology:
Cefuroxime is bactericidal, working through cell-wall synthesis inhibition, and is notably highly stable in the presence of beta-lactamases. Its broad activity spectrum includes Gram-positive aerobes (S. aureus, S. epidermidis, S. pneumoniae, S. pyogenes), and a wide range of Gram-negative aerobes (E. coli, H. influenzae [including ampicillin-resistant strains], Klebsiella spp., M. catarrhalis [including ampicillin- and cephalothin-resistant strains], N. gonorrhoeae [including penicillinase- and non-penicillinase-producing strains], N. meningitidis, P. mirabilis, Providencia rettgeri, Salmonella spp., Shigella spp.). It also covers many anaerobes.
Resistances include most Enterococcus spp., methicillin-resistant staphylococci, Listeria monocytogenes, Pseudomonas, Campylobacter spp., Legionella spp., Acinetobacter calcoaceticus, most Serratia spp., P. vulgaris, Clostridium difficile, and most Bacteroides fragilis.
Indications:
Cefuroxime is indicated for:
- Lower respiratory tract infections
- Urinary tract infections
- Skin and skin-structure infections
- Septicemia (blood infections)
- Meningitis
- Uncomplicated and disseminated gonococcal infections
- Bone and joint infections
It is also used for preoperative prophylaxis in clean-contaminated or potentially contaminated surgical procedures, such as vaginal hysterectomy or open heart surgery.
Actionable Insights for Cefuroxime (Parenteral): - Concomitant Therapy: Cefuroxime may be used concomitantly with an aminoglycoside, particularly in cases of sepsis or when the causative organism is yet to be identified, to provide broader empiric coverage.
- S. pyogenes Duration: For S. pyogenes infections, therapy must be a minimum of 10 days to prevent sequelae.
- Surgical Drainage: As with other severe infections, surgical drainage should be performed where indicated for collections of pus.
Dosage & Administration (IV/IM): - Adults: The usual range is 750 mg to 1.5 grams every 8 hours for 5-10 days.
- Uncomplicated UTI, Skin/Skin-structure, Disseminated Gonococcal, Uncomplicated Pneumonia: 750 mg every 8 hours.
- Severe/Complicated infections, Bone/Joint: 1.5 grams every 8 hours.
- Life-threatening/less susceptible infections: 1.5 grams every 6 hours.
- Bacterial Meningitis: Maximum 3 grams every 8 hours.
- Uncomplicated Gonococcal (IM): A single 1.5-gram dose (administered at two different sites) plus 1 gram of oral probenecid.
- Adults (Prophylaxis):
- General Surgery: 1.5 grams IV just before surgery. If the procedure is prolonged, repeat with 750 mg IV/IM every 8 hours (stop within 24 hours).
- Open Heart Surgery: 1.5 grams IV at the induction of anesthesia and every 12 hours thereafter for a total of 6 grams (continue for at least 48 hours post-op).
- Pediatric (>3 months): 50-100 mg/kg/day in equally divided doses every 6 to 8 hours. Higher dosages (100 mg/kg/day, up to the maximum adult dose) may be used for severe infections.
- Bone/Joint: 150 mg/kg/day in equally divided doses every 8 hours (up to the maximum adult dose).
- Bacterial Meningitis: 200-240 mg/kg/day IV in divided doses every 6 to 8 hours.
Renal Dosing (Adults, based on CrCl): - CrCl > 20 mL/min: 750 mg to 1.5 grams every 8 hours.
- CrCl 10-20 mL/min: 750 mg every 12 hours.
- CrCl < 10 mL/min: 750 mg every 24 hours.
- Hemodialysis: Administer a further dose at the end of dialysis.
Cefuroxime axetil (Ceftin® - Oral): Bridging Hospital to Home Care
Cefuroxime axetil (Ceftin®) is the oral prodrug form of cefuroxime, offering the convenience of oral administration for milder to moderate infections, often as a step-down therapy from intravenous cefuroxime.
Actionable Insights for Cefuroxime Axetil:
- Bioequivalence Warning: This is critical: CEFTIN TABLETS AND ORAL SUSPENSION ARE NOT BIOEQUIVALENT AND ARE NOT SUBSTITUTABLE ON A MILLIGRAM-PER-MILLIGRAM BASIS. This means you cannot simply switch between the two formulations without a new prescription and dosage adjustment.
- S. pyogenes Sensitivity: For S. pyogenes infections, the pathogen must be sensitive to both penicillin and cefuroxime for effective treatment.
Indications (Tablets - Adolescents/Adults 13+):
Ceftin tablets are indicated for mild to moderate infections, including: - Pharyngitis/tonsillitis (S. pyogenes)
- Acute bacterial otitis media (S. pneumoniae, H. influenzae [including beta-lactamase-producing strains], M. catarrhalis [including beta-lactamase-producing strains], S. pyogenes)
- Acute bacterial maxillary sinusitis (S. pneumoniae or H. influenzae non-beta-lactamase strains only)
- Acute bacterial exacerbations of chronic bronchitis and secondary bacterial infections of acute bronchitis
- Uncomplicated skin and skin-structure infections
- Uncomplicated urinary tract infections
- Uncomplicated gonorrhea
- Early Lyme disease (Borrelia burgdorferi)
Indications (Oral Suspension - Pediatric 3 months-12 years):
The oral suspension is indicated for mild to moderate infections in this age group, including: - Pharyngitis/tonsillitis (S. pyogenes)
- Acute bacterial otitis media (S. pneumoniae, H. influenzae [including beta-lactamase-producing strains], M. catarrhalis [including beta-lactamase-producing strains], S. pyogenes)
- Impetigo (S. aureus [including beta-lactamase-producing strains], S. pyogenes)
Dosage & Administration:
(Note: The provided context research for Cefuroxime axetil dosage information abruptly cuts off. As per instructions to only use provided ground truth, I can only state what was given, and will make a note of the truncation.) - Ceftin Tablets (Adolescents/Adults 13+): May be administered without regard to meals.
- Pharyngit... (Information incomplete in provided context).
Further specific dosage information for Cefuroxime axetil, particularly for different indications and pediatric populations, was not fully provided in the context research. Always refer to a complete drug reference or consult a healthcare professional for precise dosing guidelines.
Important Considerations for Prescribing and Using 2nd Gen Cephalosporins
Beyond the specific indications and dosages, there are overarching considerations that apply to the entire class of second-generation cephalosporins.
Understanding Potential Side Effects
While generally well-tolerated, like all medications, second-generation cephalosporins can cause side effects. Most are mild and resolve quickly, often within 1-2 days.
Common Side Effects:
- Stomach discomfort
- Nausea
- Vomiting
- Decreased appetite
- Dizziness
- Skin rash
- Diarrhea
- Yeast infections (oral or vaginal)
- Increased liver enzymes (often transient and asymptomatic)
Rare but Serious Side Effects: - Hypersensitivity Reactions: These can range from mild rashes to severe, life-threatening anaphylaxis. Always screen patients for penicillin or cephalosporin allergies before administration.
- Difficulty Breathing: Can be a sign of a severe allergic reaction.
- Low Blood Pressure (Hypotension): Especially with rapid IV administration.
- Thrombocytopenia: A decrease in platelet count, leading to increased bleeding risk.
- Fever: Can sometimes be drug-induced.
- Drug-Induced Immune Hemolytic Disease: A very rare but serious condition where the body's immune system attacks its own red blood cells due to the drug.
Renal Impairment: A Key Adjustment Factor
Most second-generation cephalosporins are primarily excreted by the kidneys. This means that for patients with impaired renal function (kidney disease), dosages often need to be adjusted to prevent accumulation of the drug and potential toxicity. Referencing specific drug guidelines based on creatinine clearance (CrCl) or estimated glomerular filtration rate (eGFR) is crucial for safe and effective treatment.
When to Exercise Caution or Avoid Use
- Allergies: A known hypersensitivity or severe allergic reaction to penicillin or other cephalosporins is a contraindication. Cross-reactivity between penicillins and cephalosporins, while less common with newer cephalosporins, still warrants careful consideration.
- Resistant Organisms: As outlined in the microbiology sections, these drugs are not effective against all bacteria. Using them against known resistant pathogens can lead to treatment failure and contribute to antibiotic resistance.
- C. difficile Infection: Like most broad-spectrum antibiotics, cephalosporins can disrupt normal gut flora, potentially leading to Clostridioides difficile-associated diarrhea (CDAD), which can range from mild to life-threatening.
Monitoring During Therapy
Depending on the specific drug and patient's condition, monitoring may include:
- Clinical Response: Improvement in symptoms (fever, pain, inflammation).
- Laboratory Tests: Complete blood counts (CBC), renal function tests (creatinine, BUN), and liver function tests (LFTs), especially with prolonged therapy or in patients with pre-existing conditions.
- Culture and Sensitivity: If initial empiric therapy is given, confirming the pathogen's susceptibility is vital to ensure the chosen antibiotic is appropriate.
Navigating the Landscape of Antibiotics: FAQs
Are second-generation cephalosporins "better" than first-generation ones?
It's not about being "better," but different. Second-generation cephalosporins offer an expanded spectrum of activity, particularly against Gram-negative bacteria like Haemophilus influenzae and Klebsiella pneumoniae, which first-generation agents might not cover as effectively. First-generation cephalosporins, however, generally retain stronger activity against Gram-positive organisms, especially Staphylococcus aureus (methicillin-susceptible) and Streptococcus pyogenes. The choice depends entirely on the suspected or confirmed pathogen and the infection site.
What about third-generation cephalosporins? How do they compare?
Third-generation cephalosporins generally offer even broader Gram-negative coverage than second-gens, often including more resistant Gram-negative bacilli, but typically have reduced Gram-positive activity compared to first and second generations. They are often reserved for more serious or resistant infections.
Can I take oral second-generation cephalosporins with food?
This varies by specific drug. Some, like cefuroxime axetil tablets, can be taken without regard to meals. Others might have improved absorption when taken with food, or conversely, decreased absorption. Always check the specific drug instructions or consult your pharmacist.
What if I miss a dose?
If you miss a dose, take it as soon as you remember, unless it's almost time for your next scheduled dose. In that case, skip the missed dose and resume your regular dosing schedule. Do not double up doses to make up for a missed one. Consistency is key for antibiotic effectiveness.
How concerned should I be about antibiotic resistance with these drugs?
Antibiotic resistance is a global health concern for all antibiotic classes, including second-generation cephalosporins. Overuse or misuse contributes to resistance. It's crucial to use these medications only when indicated, at the correct dosage, and for the full prescribed duration, even if you feel better. This helps ensure the bacteria are fully eradicated and reduces the chance of resistant strains developing.
Moving Forward with Confidence: The Enduring Role of 2nd Gen Cephalosporins
Second-generation cephalosporins hold a firm and well-deserved place in antimicrobial therapy. Their balanced spectrum of activity, particularly their strength against key Gram-negative pathogens and, for some, anaerobes, makes them indispensable for a wide array of infections. From routine upper respiratory issues to complex surgical prophylaxis and severe deep-seated infections, these drugs provide effective and targeted treatment options.
However, intelligent use is paramount. Prescribing the right drug for the right bug, considering patient factors like renal function and allergies, and adhering to appropriate dosing and duration are not just best practices – they are critical to preserving the efficacy of these valuable medications. As bacteria continue to evolve, so too must our approach to antibiotics, leaning on expert knowledge and careful consideration to ensure second-generation cephalosporins remain potent tools for future generations. Always work closely with your healthcare provider to make informed decisions about your antibiotic treatment.