In the ongoing battle against bacterial infections, having the right antibiotic is like wielding the perfect tool for a specific job. Among the diverse arsenal of antimicrobial agents, Specific 2nd Generation Cephalosporin Drugs & Spectrum stand out as versatile, broad-spectrum options that bridge the gap between their predecessors and more advanced cousins. These medications are not just another class of antibiotics; they represent a crucial advancement in targeting a wider array of bacteria, making them indispensable in various clinical scenarios.
From common respiratory ailments to complex intra-abdominal infections, understanding which specific drugs fall into this category and precisely what bacteria they target is key to effective treatment.
At a Glance: Your Quick Guide to 2nd-Gen Cephalosporins
- What they are: A group of bactericidal, broad-spectrum antibiotics, part of the cephalosporin family, discovered after 1945.
- How they work: They kill bacteria by disrupting the formation of their protective cell walls.
- Key advantage: Enhanced activity against many gram-negative bacteria compared to first-generation cephalosporins, while retaining some gram-positive coverage. They also offer improved anaerobic coverage in some subgroups.
- Common uses: Treating infections of the bones, joints, skin, urinary tract, respiratory tract, and certain gynecological and abdominal infections. Some can even tackle meningitis in children.
- Important considerations: Often reserved when penicillins aren't suitable. Be aware of potential side effects, including a cross-reactivity risk with penicillin allergies.
The Unseen Battle: How 2nd-Gen Cephalosporins Target Bacteria
Imagine bacteria as tiny, walled fortresses. Their walls, made of a unique substance called peptidoglycan, are essential for their survival, providing structural integrity and protection. Without these walls, the bacteria are vulnerable and quickly succumb. This is precisely where second-generation cephalosporins shine.
These antibiotics, derived from the Acremonium mold, are bactericidal, meaning they actively kill bacteria rather than just inhibiting their growth. Their modus operandi is quite elegant: they bind to and block specific enzymes (known as penicillin-binding proteins) that are crucial for creating peptidoglycan. By halting this vital construction process, they compromise the bacterial cell wall, leading to its lysis (rupture) and, ultimately, the death of the bacterial cell. It's a highly effective strategy that has saved countless lives.
Moving Beyond the First Line: Why Second-Gen Cephalosporins Are Different
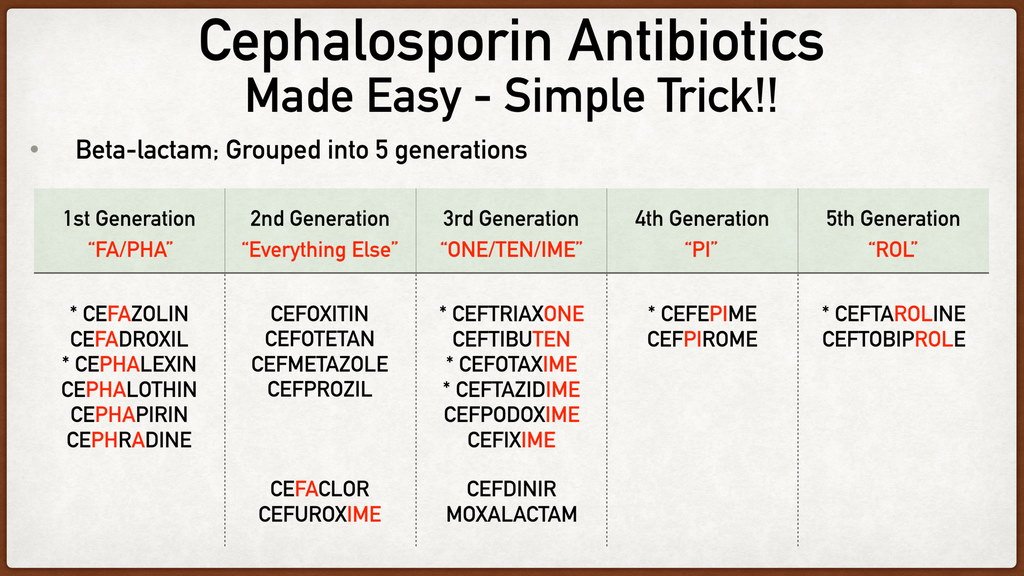
The world of cephalosporins is organized into five "generations," each building upon the last with subtle yet significant shifts in their spectrum of activity. Second-generation cephalosporins mark a distinct evolution from their first-generation counterparts.
While first-generation cephalosporins are excellent against many gram-positive bacteria (like staphylococci and streptococci), they have more limited action against gram-negative organisms. Second-generation drugs flip this script somewhat: they offer increased activity against gram-negative bacteria, making them effective against a broader range of tricky pathogens. However, this comes with a slight trade-off: their efficacy against gram-positive bacteria is generally less pronounced than that of the first generation. This strategic shift makes them valuable tools for specific types of infections where gram-negative culprits are more common.
If you're interested in the broader family of these vital medications, you might want to Explore second-generation cephalosporins further to understand their place in antimicrobial therapy.
Meet the Team: Specific 2nd Generation Cephalosporin Drugs You'll Encounter
When we talk about specific 2nd generation cephalosporin drugs, we're referring to a handful of agents that have proven their worth in clinical practice. Each has its own nuances, but they share the core characteristics of their generation.
The most commonly used and recognized examples include:
- Cefaclor (e.g., Ceclor)
- Cefotetan (e.g., Cefotan)
- Cefoxitin
- Cefprozil (e.g., Cefzil)
- Cefuroxime (e.g., Ceftin, Zinacef)
It's also worth noting that some 2nd-generation cephalosporins, such as cefamandole, cefmetazole, cefonicid, and loracarbef, have been discontinued over time due to various factors, including the development of newer drugs, resistance patterns, or evolving clinical preferences.
Within this generation, there are also important subgroups that fine-tune their bacterial targeting: - Cefuroxime and Cefprozil: These agents offer particularly increased coverage against Haemophilus influenzae, a common cause of respiratory infections, otitis media, and meningitis.
- The Cephamycin Subgroup: This unique group includes drugs like cefoxitin and cefotetan. What sets them apart is their significantly increased coverage against anaerobes, most notably Bacteroides species. This makes them especially valuable for treating infections where anaerobic bacteria are known to play a role, such as intra-abdominal or gynecological infections.
Pinpointing the Enemy: The Bacterial Spectrum of 2nd-Gen Cephalosporins
Understanding the "spectrum" of an antibiotic means knowing exactly which types of bacteria it's effective against. For 2nd-generation cephalosporins, this spectrum is notably broad, making them go-to choices for a variety of infections.
Gram-Negative Aerobes: Expanding the Reach
This generation truly shines against a range of gram-negative aerobic bacteria, which are often implicated in more challenging infections. You'll find them effective against:
- Morganella morganii
- Non-penicillinase producing Neisseria gonorrhoeae (important for certain sexually transmitted infections)
- Haemophilus influenzae (a common culprit in ear infections, sinusitis, and bronchitis)
- Klebsiella species (can cause pneumonia, UTIs)
- Escherichia coli (a frequent cause of UTIs and other infections)
The enhanced activity against these pathogens is a key differentiator from the first generation.
Gram-Positive Aerobes: Still a Strong Contender
While their gram-positive activity is generally considered less robust than first-gen drugs, 2nd-generation cephalosporins still provide good coverage against several important gram-positive aerobes, including:
- Streptococcus pneumoniae (a major cause of pneumonia and meningitis)
- Staphylococcus aureus (excluding MRSA, which is methicillin-resistant S. aureus)
- Staphylococcus epidermidis
- Streptococcus pyogenes (the cause of strep throat and other skin infections)
Anaerobes: The Hidden Threat
One of the most valuable aspects of the cephamycin subgroup (cefoxitin, cefotetan) is their efficacy against anaerobic bacteria. These organisms thrive in oxygen-poor environments and are often found in mixed infections, particularly in the abdomen and pelvis. Key anaerobic targets include:
- Bacteroides species (especially Bacteroides fragilis, a significant pathogen in intra-abdominal infections)
- Other anaerobes commonly found in the gut.
The Resistant Foes: Know Their Limits
No antibiotic is a silver bullet, and 2nd-generation cephalosporins have their limitations. It's crucial for healthcare providers to be aware of the bacteria that are typically resistant to these drugs. Most strains of:
- Pseudomonas aeruginosa
- Acinetobacter species
are resistant. These highly resistant gram-negative bacteria often require different, more potent antibiotics for effective treatment. This highlights the importance of accurate diagnosis and susceptibility testing.
Where These Drugs Make a Difference: Clinical Applications
Given their broad and specific spectrum, second-generation cephalosporins are used to treat a diverse array of infections. They are typically reserved for situations where first-line antibiotics, such as penicillins, either cannot be used (due to allergy or resistance) or are simply not as effective for the suspected pathogen.
Common clinical applications include:
- Bone and Joint Infections: Such as osteomyelitis or septic arthritis, often caused by staphylococci or streptococci, where effective penetration into these tissues is crucial.
- Gynecological Infections: Including pelvic inflammatory disease or endometritis, where mixed aerobic and anaerobic flora are common, making the cephamycin subgroup particularly useful.
- Intra-abdominal Infections: Peritonitis, diverticulitis, or other infections within the abdominal cavity, frequently involving a mix of gram-negative aerobes and anaerobes. Cefoxitin and cefotetan are often chosen here.
- Lower Respiratory Tract Infections: Such as bronchitis, community-acquired pneumonia, or exacerbations of chronic obstructive pulmonary disease, especially when H. influenzae or S. pneumoniae are suspected. Cefuroxime is a frequent choice.
- Skin and Skin Structure/Soft Tissue Infections: Including cellulitis or abscesses, particularly those caused by staphylococci or streptococci, or in cases where gram-negative involvement is a concern.
- Urinary Tract Infections (UTIs): Especially those complicated by specific gram-negative bacteria or when other antibiotics are ineffective.
- Meningitis (in Children): Cefuroxime has historically been used for bacterial meningitis in children, demonstrating its ability to cross the blood-brain barrier.
- Blood Infections (Sepsis): When caused by susceptible organisms, these drugs can be part of the treatment regimen to control systemic infections.
Navigating the Side Effects: What to Expect and When to Be Cautious
Second-generation cephalosporins are generally considered safe, with low toxicity and good efficacy when used appropriately. However, like all medications, they can cause side effects. Awareness is key to managing treatment effectively.
Common Side Effects: Often Mild and Transient
Many people experience minor side effects that often resolve within 1 to 2 days of starting therapy. These can include:
- Abdominal pain or stomach discomfort
- Nausea
- Vomiting
- Diarrhea
- Skin rash
- Decreased appetite
- Dizziness
- Transient increases in liver enzymes (usually not clinically significant)
Serious Side Effects: Rare, But Demand Attention
While uncommon, some serious side effects can occur and require immediate medical attention:
- Allergic Reactions: Ranging from severe skin rashes and hives to swelling (angioedema) and even life-threatening anaphylaxis. It's critical to inform your doctor about any known drug allergies, especially to penicillins. Up to 10% of individuals with a penicillin allergy may also experience an allergic reaction to cephalosporins, a phenomenon known as cross-reactivity.
- Drug-Induced Immune Hemolytic Disease/Anemia: A rare condition where the drug triggers the immune system to destroy red blood cells, leading to anemia.
- Super-infection due to Clostridium difficile (C. diff): Antibiotics can disrupt the normal balance of gut bacteria, allowing C. difficile to overgrow. This can lead to severe diarrhea, abdominal pain, and in serious cases, life-threatening colon inflammation.
- Seizures: This is a rare side effect, with an increased risk in individuals with pre-existing kidney disease, as the drug may accumulate to higher levels.
- Thrombocytopenia: A decrease in the number of platelets in the blood, which can increase the risk of bleeding.
- Low Blood Pressure (Hypotension)
- Difficulty Breathing
Important Considerations and FAQs
Are all 2nd-gen cephalosporins the same?
Absolutely not. While they share generational characteristics, individual drugs within this class have distinct pharmacokinetic properties (how the body handles them) and subtle differences in their spectrum of activity. For instance, cefoxitin and cefotetan (the cephamycins) have superior anaerobic coverage compared to cefaclor or cefuroxime. Your doctor will choose the specific drug best suited for your infection based on the likely pathogen, the site of infection, and your individual health profile.
Can I take a 2nd-gen cephalosporin if I'm allergic to penicillin?
This is a critical conversation to have with your healthcare provider. While there's a risk of cross-reactivity (up to 10%), it's not a universal contraindication. For patients with a mild penicillin allergy (e.g., a rash), some cephalosporins might be cautiously administered. However, if you have a history of a severe penicillin allergy (e.g., anaphylaxis), cephalosporins are generally avoided, and alternative antibiotic classes would be considered. Always be upfront about your allergy history.
What's the main difference between 1st and 2nd generation cephalosporins?
The primary distinction lies in their bacterial spectrum. First-generation cephalosporins offer excellent coverage against gram-positive bacteria (like many staph and strep strains) but limited gram-negative activity. Second-generation drugs shift this balance, providing more potent activity against many gram-negative aerobes (like H. influenzae, E. coli, Klebsiella) and, in some cases, good anaerobic coverage, while slightly reducing their overall gram-positive prowess compared to the first generation.
Why are some 2nd-gen cephalosporins discontinued?
Drug discontinuations can happen for various reasons. It could be that newer, more effective, or safer antibiotics emerged, rendering older ones less competitive. Increased bacterial resistance to a particular drug can also reduce its clinical utility. Sometimes, market factors, manufacturing complexities, or even the rare discovery of unexpected adverse effects can lead to a drug being pulled from the market.
Your Role in Smart Antibiotic Use: Making Informed Decisions
Understanding specific 2nd generation cephalosporin drugs and their bacterial spectrum empowers you to be a more informed participant in your healthcare. These medications are powerful tools, but they require careful and judicious use.
Always:
- Communicate Clearly: Tell your doctor about all your medical conditions, medications you're taking, and especially any known allergies (particularly to penicillin).
- Adhere to the Regimen: Take your antibiotic exactly as prescribed – don't skip doses, and complete the entire course, even if you start feeling better. Stopping early can lead to recurrence and contribute to antibiotic resistance.
- Report Side Effects: Don't hesitate to inform your doctor or pharmacist if you experience any unusual or severe side effects. They can help manage them or adjust your treatment.
- Ask Questions: If anything about your medication or treatment plan is unclear, ask! Your healthcare team is there to guide you.
The judicious use of antibiotics like 2nd-generation cephalosporins is vital not only for your health but for public health in the larger fight against antimicrobial resistance. By understanding their strengths and limitations, we can ensure these valuable drugs continue to be effective for generations to come.